GI and Diabetes
There is strong evidence that low GI diets decrease the risk of type 2 diabetes and improve the management of diabetes.

The facts at a glance
Diabetes is a chronic condition where a person has high blood glucose levels in their blood. When you don’t have enough insulin to convert food into energy, the glucose stays in the blood.
An estimated 552 million people will have diabetes by 2030. It’s the world’s fastest growing chronic disease. Around 80% of people with diabetes will die from a heart attack or stroke.
A low GI diet improves glucose levels, reduces insulin resistance and improves blood cholesterol, which are all important for managing diabetes and reducing the risk of long-term complications.
ON THIS PAGE
PRINT, DOWNLOAD, SHARE
About diabetes
Diabetes is a chronic condition in which a person has high glucose levels (sometimes called blood sugar) in their blood. For our bodies to function properly, we need to convert glucose (sugar) from food into energy.
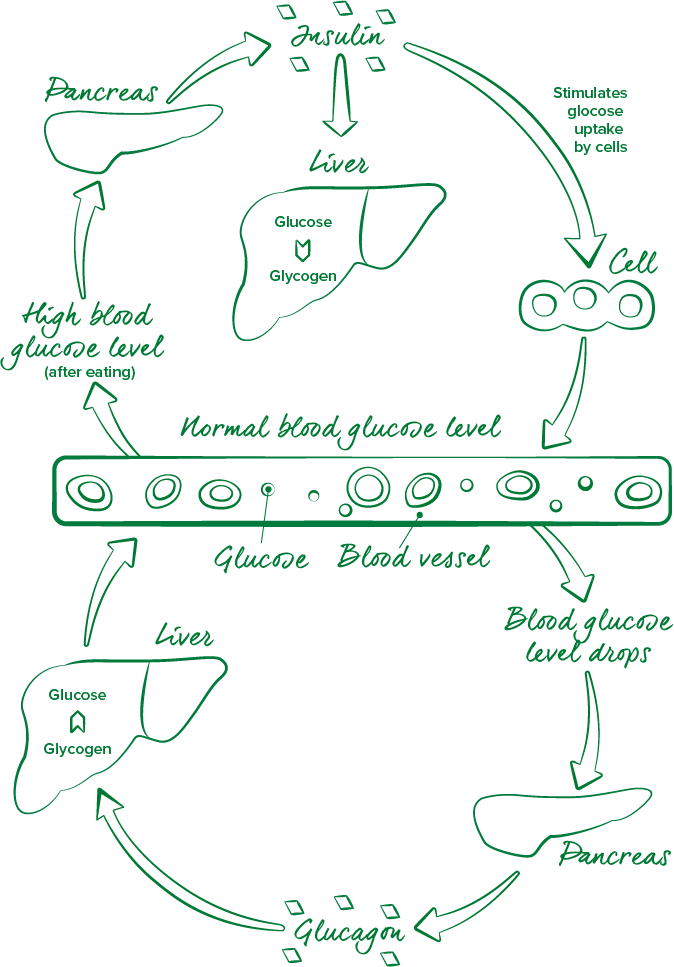
To understand diabetes, it’s helpful to know the basics of how the body metabolises (breaks down) blood glucose. When you eat carbohydrate – such as a bowl of cereal, pasta or fruit – the digestive system breaks down the carbohydrate into glucose (simple sugars) which travels through the bloodstream to energise cells.
Insulin is released by the beta cells in response to the rise in blood glucose levels after eating. Insulin directs the glucose into the liver and muscle cells, promoting the storage of nutrients and preventing your blood glucose levels to rise excessively.
In people with diabetes, insulin is no longer produced, or not produced in sufficient amounts, by the body. Instead of being turned into energy, the glucose stays in the blood which results in high blood glucose levels.
In a person who is overweight or obese, the cells of the body become less responsive to insulin, which in turn causes the body to secrete more insulin to maintain normal metabolism. For some people, however, the insulin producing cells fail to keep up with this demand, and thus leads to type 2 diabetes.
The main types of diabetes
Type 1:
Type 1 diabetes usually develops in childhood or adolescence, but can also develop in adulthood. It occurs when the immune system mistakenly attacks and kills the beta cells of the pancreas, meaning no, or very little, insulin is released into the body. As a result, blood glucose builds up in the blood instead of being used as energy. Type 1 diabetes is always treated with insulin, but meal planning also helps with keeping blood glucose at the right levels. About 5-10% of people with diabetes have type 1.
Type 2:
Type 2 diabetes accounts for 85% of all diabetes. It is a progressive condition in which the body becomes resistant to the normal effects of insulin and/or gradually loses the capacity to produce enough insulin in the pancreas. It is one of the major consequences of the obesity epidemic around the world due to changes in diet and a less active lifestyle. It also has strong genetic and family related risk factors.
Gestational (sometimes referred to as GDM):
Gestational diabetes is a temporary condition that is diagnosed when higher than normal blood glucose levels first appear during pregnancy. It affects approximately 5-10% of all pregnancies. Once the pregnancy is over and blood glucose levels return to normal, the diabetes disappears. However, this insulin resistance increases the risk of developing type 2 diabetes in later life.
Pre-diabetes:
A condition in which blood glucose levels are higher than normal, although not high enough to be diagnosed as type 2 diabetes. Pre-diabetes has no signs or symptoms. Without sustained lifestyle changes, including healthy eating, increased activity and losing weight, approximately one in three people with pre-diabetes will go on to develop type 2 diabetes and have a higher risk of developing cardiovascular (heart and circulation) disease.
1.3
million
Australians live with diabetes and a further 500,000 are undiagnosed
700
million
people globally will have diabetes by 2045
80%
of people with diabetes will die from a heart attack or stroke
Source: International Diabetes Federation and Diabetes NSW
How a low GI lifestyle can help
Studies around the world show that following a low GI diet significantly helps people with diabetes improve their blood glucose levels and can reduce the risk of developing type 2 diabetes. Strong evidence suggests that type 2 diabetes can be prevented in up to 58% of cases in the high risk (pre-diabetes) population by eating well and exercising.
Low GI diets have been shown to:
- Improve blood glucose levels by reducing blood glucose spikes
- Reduce insulin resistance
- Help people with diabetes reduce their HbA1c by 0.5%
- Help decrease the risk of common diabetic complications by ~20%
- Improve blood cholesterol levels, particularly LDL cholesterol
- Increase feelings of fullness after eating and reduce hunger between meals
- Increase the rate of weight loss and reduce waist circumference
- Help prevent weight regain over the longer term
- Reduce the risk of vascular disease
Strong evidence shows that type 2 diabetes can be prevented in up to 58% of cases in the high risk (pre-diabetes) population by eating well and exercising
Source: Knowler WC, Barret-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393-403.
Low GI lifestyle tips
Lifestyle changes are important when managing your diabetes. Enjoying healthy foods and being active are the best first steps to implement change, however stopping smoking, getting enough sleep and eating mindfully will also help to manage blood glucose levels and body weight.
For a person with diabetes there is no need to prepare separate meals or buy special foods. It’s about simple low GI swaps, smart lifestyle choices and self-care to help maintain a healthy weight.
- Make the switch to low GI foods and look to reduce the overall GI and GL (glycemic load) of your meal
- Keep carbohydrate portions moderate at each meal and aim for ‘the ideal plate’. Half the plate should be vegetables, a quarter should be healthy low GI carbohydrates, and the final quarter filled with lean protein
- Spread consumption of carbohydrate-rich foods evenly throughout the day
- Small regular meals can help maintain energy levels, manage appetite and keep blood glucose levels within the target range
- Exercise regularly, aiming for at least 30-60 minutes of moderate exercise every day. Weight bearing exercises such as walking will also help you build strong bones and strengthen your muscles so they burn fat more efficiently
- Losing 5-10% of your body weight has been shown to help manage blood glucose control
It is important to recognise that everyone’s needs are different. All people with diabetes should see an Accredited Practising Dietitian in conjunction with their diabetes team for individualised advice.
Low GI diabetes food checklist to help control blood glucose levels
- Try to incorporate at least one low GI food at every meal
- Balance meals with healthy carbohydrates, lean protein and plenty of salad or vegetables
- Snack on fruit and non-starchy vegetables
- Eat wholegrain and high fibre cereals, breads and grains daily
- Eat at least three cups (300g) of vegetables every day
- Eat at least two pieces (200g) of fruit every day and include at least one low GI choice
- Include legumes (canned or dried peas, beans or lentils) in your diet at least twice a week
- Choose lower fat dairy products (or calcium-enriched alternatives)
- Try to include a protein-rich food at every meal
- Choose healthy ‘good fats’ that are rich in poly and mono unsaturated fats such as olive oil, avocado and unsalted nuts and seeds
- Eat fish (100g or more) at least twice a week
- Eat lean red meat and poultry in moderately sized 100g portions three or four times a week
- If you drink alcohol, drink no more than two standard drinks per day
- Drink six to eight glasses of water every day
Research and further reading
A 2019 review of 54 studies concluded that low GI diets reduced haemoglobin A1C (a long-term marker of blood sugar control), body weight, and fasting blood sugar levels in people with prediabetes or diabetes1.
What’s more, some research has linked high GI diets with a greater risk of developing type 2 diabetes. One study in over 205,000 people found that those with the highest GI diets had up to a 33% greater risk of developing type 2 diabetes than those who consumed the lowest GI diets2.
- Low-glycemic index diets as an intervention for diabetes: a systematic review and meta-analysis
- High GI diets may significantly increase type 2 diabetes risk
- Dietary glycemic index and load and the risk of type 2 diabetes: assessment of causal relations
- Low glycaemic index, or low glycaemic load, diets for diabetes mellitus
- Dietary substitutions for refined carbohydrate that show promise for reducing risk of type 2 diabetes in men and women
- Prevention and management of type 2 diabetes: dietary components and nutritional strategies
- Is there a dose-response relation of dietary glycemic load to risk of type 2 diabetes? Meta-analysis of prospective cohort studies
- Effects of different protein content and glycaemic index of ad libitum diets on diabetes risk factors in overweight adults: the diogenes multicentre, randomized, dietary intervention trial
- Low glycaemic index, or low glycaemic load, diets for diabetes mellitus
- Can a low-glycemic index diet reduce the need for insulin in gestational diabetes mellitus? A randomized trial
- Carbohydrates, glycemic index, and pregnancy outcomes in gestational diabetes
Download resources
Low GI diets can help people with diabetes reduce their HbA1c by 0.5%. This will help decrease the risk of common diabetic complications by ~20%
Recommended for you

RECIPES

GI CERTIFIED PRODUCTS
DIABETES

LOW GI LIVING

A low GI diet focuses on the quality of carbohydrates you eat. Good carbohydrates (or low GI carbohydrates) are more slowly digested helping keep your blood sugars stable, whereas bad carbohydrates cause your blood glucose levels to peak and crash. Want to know which carbohydrates are best for you? Try our swap it tool!




